Degenerative Spondylolisthesis
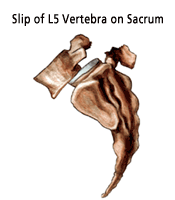
Spondylolisthesis is a spinal condition in which one vertebra slips forward over the vertebra below. Degenerative spondylolisthesis usually occurs in the lumbar spine, especially at L4-L5. It is the result of degenerative changes in the vertebral structure that cause the joints between the vertebrae to slip forward. This type of spondylolisthesis is most common among older female patients, usually those over the age of 60.
Symptoms of Degenerative Spondylolisthesis
Symptoms of spondylolisthesis may include the following:
- Pain, especially after exercise, in the low back, thighs, and/or legs that radiates into the buttocks and/or down the legs (sciatica)
- Muscle spasms
- Leg weakness
- Tight hamstring muscles
- Irregular gait or limp
Some people with spondylolisthesis are symptom free and only discover the disorder when seeing a doctor for another health problem. However, the forward slip of the vertebral body in severe cases of degenerative spondylolisthesis often leads to spinal stenosis, nerve compression, pain and neurological injury.
What Causes Degenerative Spondylolisthesis?
Degenerative spondylolisthesis is usually the result of age and "wear and tear" on the spine that breaks down vertebral components. It is different from isthmic spondylolisthesis in that there is no bone defect. Spinal stenosis tends to occur in the early stages of degenerative spondylolisthesis.
How is Spondylolisthesis Diagnosed?
Correct diagnosis is obviously essential. At our practice we utilize the latest diagnostic technologies, combined with examinations by expert physicians, to ensure that the diagnosis is accurate. Diagnostic tools include:
- Medical history. We will talk to you about your symptoms, their severity, and the treatments you have already tried.
- Physical examination. You will be carefully examined by one of our spine specialists for limitations of movement, problems with balance, pain, loss of reflexes in the extremities, muscle weakness, loss of sensation or other signs of neurological damage.
- Diagnostic tests. Generally, we start with x-rays, which allow us to rule out other problems such as tumors and infections. We may also use a CT scan or MRI to confirm the diagnosis. In some patients we may need a myelogram. This is a test that involves the use of a liquid dye that is injected into the spinal column to show the degree of nerve compression, slippage between involved vertebrae and abnormal movement.

X-Ray showing spondylolosthesis

Lumbar spine MRI showing spondylolosthesis
Classification of Spondylolisthesis
There are several methods used to "grade" the degree of slippage ranging from mild to most severe. Your surgeon will discuss with you the extent of your spondylolisthesis.
In general, the physicians at our practice use the Meyerding Grading System for classifying slips. This is a relatively easy to understand system. Slips are graded on the basis of the percentage that one vertebral body has slipped forward over the vertebral body below. Thus a Grade I slip indicates that 1-24% of the vertebral body has slipped forward over the body below. Grade II indicates a 25-49% slip. Grade III indicates a 50-74% slip and Grade IV indicates a 75%-99% slip. If the body completely slips off the body below it is classified as a Grade V slip, known as spondyloptosis.
Your physician will consider the degree of slip, and such factors as intractable pain and neurological symptoms, when deciding on the most suitable treatment. Most degenerative spondylolisthesis cases involve Grade I or Grade II. As a general guideline, the more severe slips (especially Grades III and above) are most likely to require surgical intervention.
For most cases of degenerative spondylolisthesis (especially Grades I and II), treatment consists of temporary bed rest, restriction of the activities that caused the onset of symptoms, pain/ anti-inflammatory medications, steroid-anesthetic injections, physical therapy and/or spinal bracing.
Surgery is rarely needed unless the case is severe (usually Grade III or above), neurological damage has occurred, the pain is disabling, or all non-operative treatment options have failed.
insert drawing for different degrees of spondylolisthesis
Treatment of Degenerative Spondylolisthesis
For most cases of degenerative spondylolisthesis, treatment consists of temporary bed rest, restriction of the activities that caused the onset of symptoms, pain/ anti-inflammatory medications, steroid-anesthetic injections, physical therapy and/or spinal bracing.
Degenerative spondylolisthesis can be progressive - meaning the damage will continue to get worse as time goes on. In addition, degenerative spondylolisthesis can cause stenosis, a narrowing of the spinal canal and spinal cord compression. If the stenosis is severe, and all non-operative treatments have failed, surgery may be necessary.
The most common surgical procedure used to treat spondylolisthesis is called a laminectomy and fusion. In this procedure, the spinal canal is widened by removing or trimming the laminae (roof) of the vertebrae. This is done to create more space for the nerves and relieve pressure on the spinal cord. The surgeon may also need to fuse vertebrae together. If fusion is done, various devices (like screws or interbody cages) may be implanted to enhance fusion and support the unstable spine.
We Can Help
Most people will experience some degenerative changes in their spines as they age. However, severe spondylolisthesis only affects a small percentage of the population. Overall, most degenerative disorders of the spine can be treated successfully using non-surgical methods. We will work closely with you to find a treatment method that is best for you and help you return to an active, and pain-free, lifestyle.
