Idiopathic Scoliosis
Under the direction of Dr. Akbarnia, the San Diego Center for Spinal Disorders (SDCSD), has become an internationally respected center for the treatment of idiopathic scoliosis. Dr. Akbarnia has been treating this condition for more than 3 decades, has published and taught on the subject extensively, and is still involved with the development of new treatments and technologies.
In this interview, Dr. Akbarnia provides patients with a comprehensive overview of idiopathic scoliosis.
Question: Dr. Akbarnia, can you define idiopathic scoliosis, and explain who it affects?
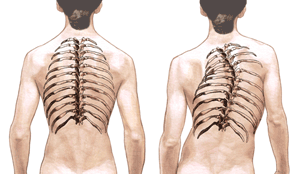
Dr. Akbarnia: Idiopathic scoliosis is a lateral (sideways) curvature of the spine that develops for unknown reasons. The curve may be to the left or to the right.
While idiopathic scoliosis can occur in young children (under the age of 10), and in adults, it is most common in adolescents (aged 10 to maturity). In fact, 3-5% of adolescents have some form of scoliosis.
In adolescents, we refer to this type of scoliosis as AIS (adolescent idiopathic scoliosis). There is undoubtedly a genetic pre-disposition for some adolescents to develop AIS, but this probably does not explain all cases. Approximately 70% of AIS patients are girls, and their curves tend to be more progressive.
Question: Does idiopathic scoliosis always need to be treated?
Dr. Akbarnia: At a minimum, idiopathic scoliosis must be carefully monitored by a spine specialist. The reason is that the condition can be progressive, and if it progresses and is left untreated it can result in significant deformity.
The deformity can have serious physical consequences. As the vertebrae (spinal bones) rotate, the rib cage is affected, which in turn can cause heart and lung compromise (i.e. shortness of breath). When progressive scoliosis affects the lumbar spine the pain can be debilitating.
In addition to the physical consequences, the deformity can cause marked psychological distress as a patient deals with the curve becoming increasingly obvious to others. The change in appearance caused by the curve, can be particularly disturbing for adolescent patients.
Question: What are the symptoms to look out for?
Dr. Akbarnia: There are several symptoms to watch for, including back pain, leg length discrepancy, an abnormal gait, and uneven hips. Patients may also notice one shoulder being higher than the other, a "prominent" shoulder blade and rib cage when bending forward, and, of course, visible curving of the spine to one side.
The first indication that patients notice is often that clothes no longer fit correctly (for example, the legs of pants may seem uneven). This is particularly common with adolescents.
Question: How do you diagnose and assess scoliosis?
Dr. Akbarnia: A comprehensive assessment must always include medical history, physical and neurological exam, and diagnostic tests.
Medical history may include questions about the parent's genealogy. Are there other family members with scoliosis? If so, how did the scoliosis progress and what treatment was provided? The physician will check for any underlying medical condition that might otherwise be causing the scoliosis. In addition, with pediatric and adolescent patients particular attention will be given the patient's age, onset of puberty, and age at which a young woman has her first period. These questions will help the physician determine the number of years that remain before the child reaches skeletal maturity. At skeletal maturity curve progression may stop as long as the curve is less than 40-45 degrees.
The curve may continue to progress throughout adulthood, if the curve exceeds 40-45 degrees. During the physical and neurological examinations the physician will learn about the patient's health and general fitness. These exams provide the physician with a "baseline" from which future curve progression can be measured. A typical examination may include the following:
| Examination | Description |
| Physical assessment | The physician looks for asymmetry of the trunk such as uneven shoulders or hips, humpback, or listing to one side. |
| Cardiopulmonary | Testing of the function of the heart and lungs. |
| Adam's Forward Bending Test |
The patient bends forward at the waist, with arms extended forward. The physician looks for asymmetry thoracic prominence (such as a shoulder blade), or a lumbar prominence. |
| Leg length | Both legs are measured to determine if they are of equal length. |
| Plumb line | A plumb line is "dropped" from the C7 vertebra (in the neck) and is allowed to hang below the buttocks. In scoliosis the line does not hang between the buttocks. |
| Range of motion | The physician measures the patient's ability to perform flexion, extension, bending, and rotation movements. |
| Palpation | The physician "feels" for abnormalities. Perhaps the ribs are more prominent on one side. |
| Neurological assessment | In addition to testing reflexes, the physician will want to know if the patient's symptoms include pain, numbness, tingling, extremity weakness or sensation, muscle spasm, and bowel/bladder changes. |
Diagnostic tests include the following:
Table 2
| Diagnostic Test | Description |
| Scoliometer | A scoliometer is used to measure a rib prominence while the patient is bent at the waist. |
| Imaging Studies | X-rays may include upright PA and lateral views of the spine and side bending or traction. MRI and CT scans may also be used, with CT Myelogram often used with adults. |
| Discograms | Only used with some adult patients and is used to help establish the pain source. |
| Cobb Angle Measurement | This test uses a full-length anterior to posterior x-ray to calculate the angle of the curve(s). |
| Risser Sign | Used with pediatric and adolescent patients. An x-ray to provide information about skeletal maturation. The Risser Sign looks at the iliac crest growth plate, a fan-shaped part of the pelvis. The crest fuses with the pelvis at maturity. The hip socket growth plate is not fully closed prior to skeletal maturity and this is also noted. |
| Nash-Moe | A technique used to measure vertebral rotation. The rotation of the vertebral pedicle is measured by dividing the vertebral body into segments. |
Question: Patients often are confused by different classification systems of scoliosis. Can you shed some light on this?
Dr. Akbarnia: Patients are not the only ones who are confused by the different classification systems, as medical professionals are sometimes confused too! However, there are a couple of simple points to keep in mind.
- Classification systems (such as King-Moe or Lenke systems) are used by doctors to help them describe curves, especially in terms of the curve pattern and magnitude. Curve pattern describes the location, number and direction of the curves. Curve magnitude describes whether a curve is structural (major) or non-structural (minor).
- Classifications can be useful as curves with similar characteristics often behave the same and respond to treatments in similar ways.
Question: Can idiopathic scoliosis be treated without surgery?
Dr. Akbarnia Some cases of idiopathic scoliosis can be treated non-surgically and others require surgical intervention.
As a general rule-of-thumb, small curves (i.e. those less than 15-20 degrees) are observed for possible progression over a period of time. At this stage, no specific treatment is needed.
With adolescent patients, larger curves (i.e. those between 20-40 degrees) will require bracing to prevent further progression of the curve. Some adolescents find wearing the brace 16 to 23 hours every day difficult. Braces can be uncomfortable, unattractive, hot, and can make a child self-conscious even though well disguised under clothing. However, when bracing works and surgery is avoided, the total commitment of patient and family required is worthwhile. At this point a carefully designed exercise program may also be recommended.
Question: Does bracing always work to stop the scoliosis in adolescents?
Dr. Akbarnia: Unfortunately, not always. Some curves do not respond to bracing. Cervicothoracic (curves from the middle of the back up into the neck) and curves greater than 40 degrees tend not to respond well to bracing. Also older patients close to skeletal maturity may not respond to bracing.
Question: If surgery is prescribed, what are the goals?
Dr. Akbarnia: Surgery may be recommended for curves in excess of 40 degrees. Surgery for scoliosis involves special surgical implants such as rods, hooks, screws, and wires. The goal is to straighten and balance the spine and secure it in place (fusion) so curve progression stops. Surgery does not cure scoliosis; it is simply a way to correct the curve and manage the progression of the disease to avoid greater deformity.
Question: What type of surgery will be performed?
Dr. Akbarnia There is not a simple answer to this question! A specific surgical plan will be developed for each person, whether a child, adolescent or adult. However, there will be common elements to most surgeries:
- The procedure will be performed from either the front of the spine (anterior), from the back (posterior) or in some cases a combined approach (one procedure from the front, and one from the back) will be performed.
- The procedure will involve an instrumented fusion, in which the goal is to fix the spine into a straighter and more balanced position. Fusions will involve the "joining" of two or more vertebrae together by inserting bone graft or bone substitutes between the vertebrae. Special surgical implants such as hooks, screws and rods will then be used to keep the spine in place until the fusion occurs over a period of months and years.
Question: Are there any new surgical techniques on the horizon?
Dr. Akbarnia: Yes, advances in surgical techniques and technologies are happening steadily. I am involved with the development of some of these new techniques, including Growth Rods. In addition, my practice uses other recent advances including minimally invasive techniques when suitable, and bone growth substitutes such as BMP's. However, I would stress that we never use a new technique or technology until we are convinced that it will be safe and more effective than current methods.
Question: After surgery, will I take long to recover?
Dr. Akbarnia: As always, the recovery process will depend on the extent of your surgery, your age and general health prior to the surgery, and several other factors. Your medical team will give you a clear description of your likely recovery process prior to the surgery. In addition, they will be available to you throughout your recovery to address any concerns or questions.
As a general guide, most patients who have undergone major scoliosis surgery can expect a recovery process that involves:
- 1-3 days post-op: You will be encouraged to get out of bed and try walking.
- 5-7 days post-op. Usually patients whose surgery went relatively smoothly will be discharged home.
- 1-8 weeks post-op. Slow return to modest activities (e.g. light walking) will be encouraged, along with good rest. Adolescents are sometimes able to return to school within 3-4 weeks of surgery, while adults are often able to return to work 6-8 weeks after surgery.
- 2 months - 1 year post-op: Fusions take at least 6 months to heal (in adolescents) and sometimes more than one year to heal in adults. Accordingly, your surgeon will monitor your progress very carefully during this time, and will instruct you on the types of activities that you can and cannot participate in.
Question: Do you have any final advice?
Dr. Akbarnia: Yes, do not hesitate to ask the medical team for advice. We understand that surgery is a major undertaking, ad we want to help you through the entire process smoothly. The better we communicate, the more likely it is that you will experience a successful outcome.
